Buruli Ulcers: a possible diagnosis in case of atypical non-healing ulcer
Image Description
Atypical ulcers (approximately 20% of ulcers) are characterized by an atypical wound bed, edges and perilesional skin (1). In order to diagnose an atypical ulcer, exclusion of typical etiologies is the first step. The clinical aspects are correlated with different etiologies. The differential diagnosis can include Pyoderma gangrenosum (Inflammatory ulcer), Calciphylaxis (Vasculopathy), Adamantinoma (Neoplastic ulcer), Mycobacteriosis (Infectious ulcer), Hydroxyurea-induced ulcer and Heroin induced ulcer (2,3).
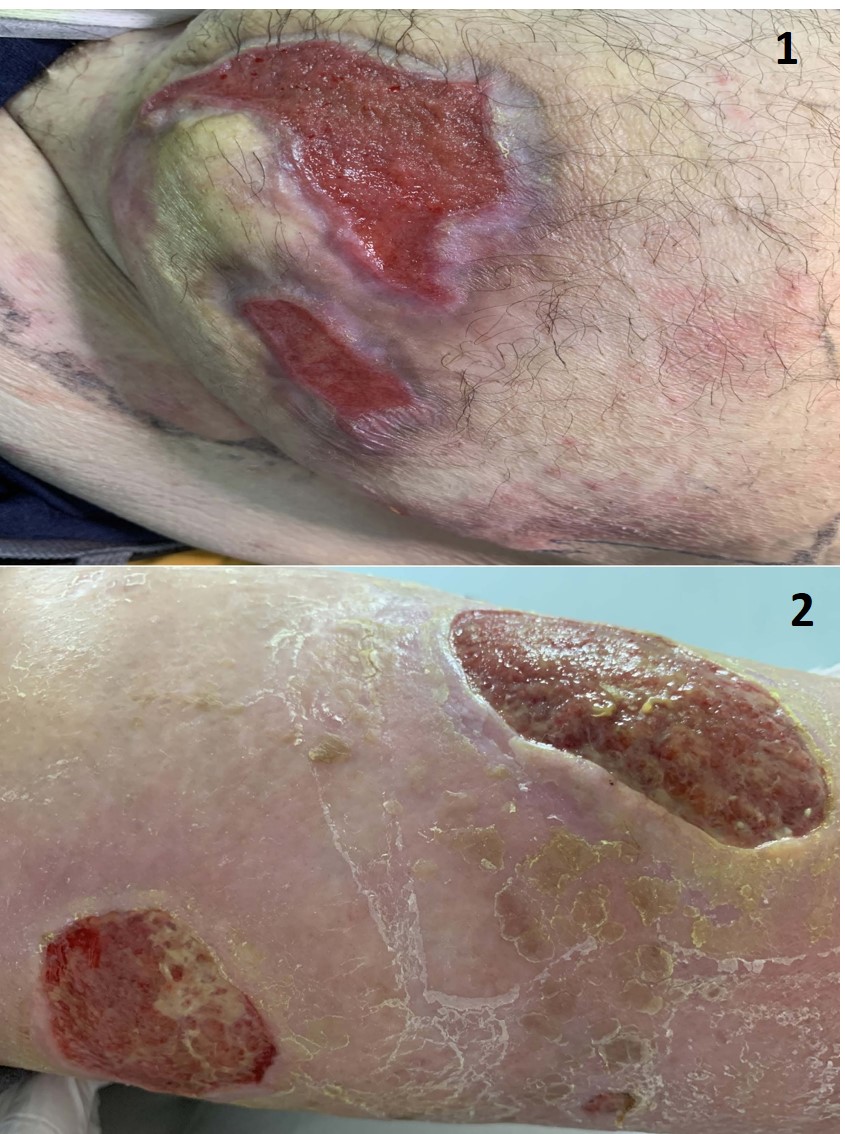
We present the case of a 59-year-old man, that presents to our department with three non-healing wounds. The wound bed is exuberant with necrotic tissue, undermined edges (lesions on the hip), vegetative with hyper-granulation tissue and well-demarcated edges (2 lesions on the lower left limb). Medical and travel (holiday in Tanzania 1-month prior to lesions onset) history and physical examination suggest additional investigations. Histological evaluation differentiates between neoplastic, vascular or inflammatory ulcers, and in our case, histology shows an inflammatory ulcer and acid-fast bacilli typically appear in clusters on the Ziehl–Neelsen stain. So, the diagnosis is Buruli ulcer.
Buruli ulcer, caused by Mycobacterium ulcerans, is a chronic debilitating disease that affects mainly the skin and sometimes the bone. The organism belongs to the family of bacteria that causes tuberculosis and leprosy, but M. ulcerans is an environmental bacterium and produces a unique toxin – mycolactone. The mode of transmission to humans remains unknown. Early diagnosis and treatment are crucial to minimizing morbidity, costs and preventing long-term disability. Treatment includes anti-mycobacterial antibiotics (rifampicin, streptomycin, amikacin) that are able to kill M. ulcerans in human lesions (4).
References
Hofman MD. Atypical ulcers. Dermatol Ther. 2013;26:222–223.
Shelling ML, Federman DG, Kirsner RS. Clinical approach to atypical wounds with a new model for understanding hypertensive ulcers. Arch Dermatol. 2010;146:1026–1029.
Isoherranen K, O’Brien JJ, Barker J, et al. Atypical wounds. Best clinical practice and challenges. J Wound Care. 2019;28(Sup6):S1–S92.
World Health Organization (2003) Buruli ulcer disease: Mycobacterium ulcerans infection. Wkly Epidemiol Rec 78: 163–168.