Fetal annexes’ changes in chorioamnionitis and premature rupture of membranes
Image Description
Premature rupture of membranes has an incidence of five to ten percent of all deliveries [1,2]. Its multifactorial cause includes a structural defect in the membranes due to malformations or collages deficiency, membranes weakness due to inflammatory or infectious processes, or cervical incompetence [1].
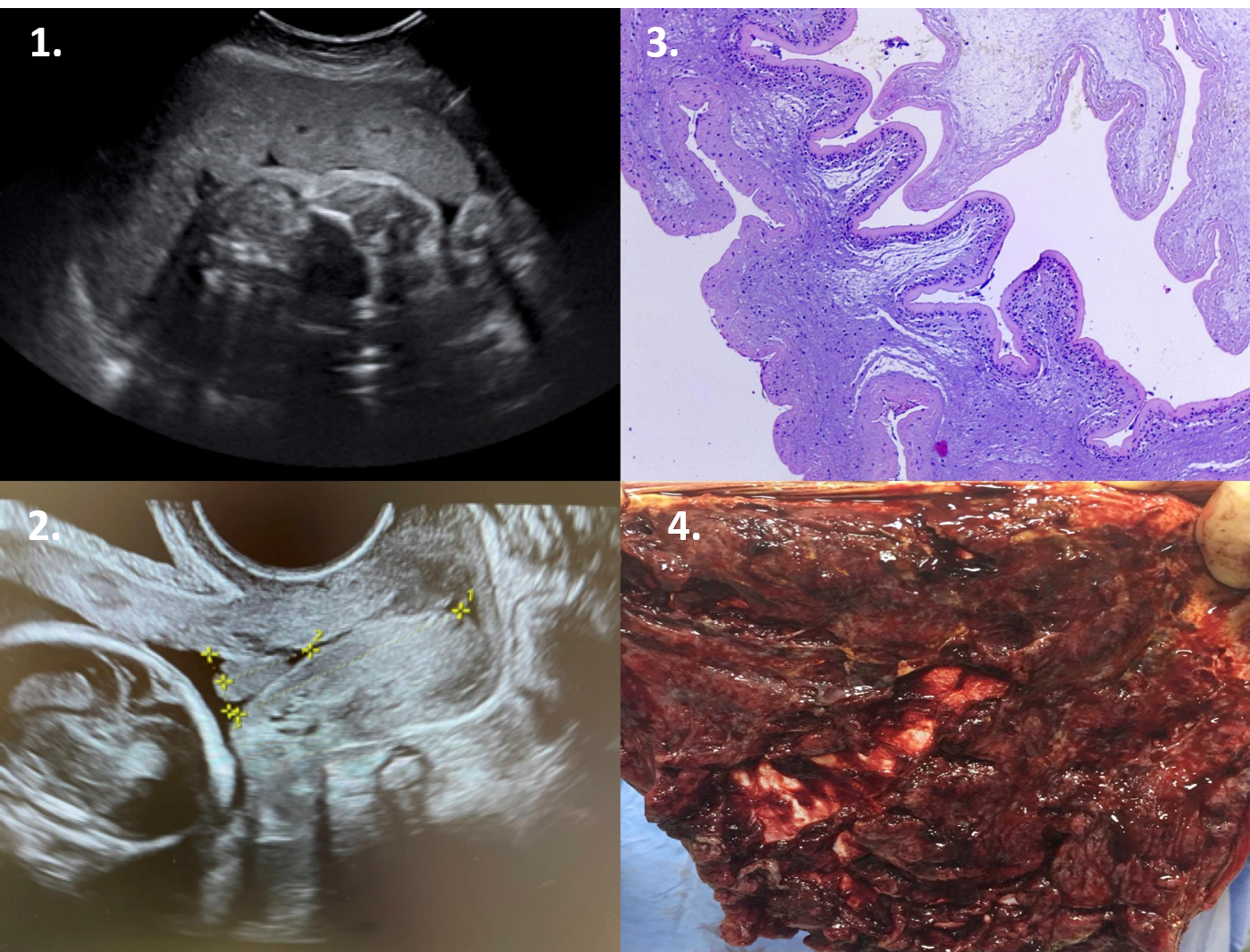
In the patients we monitored, we observed that 20 percent of the patients with cervical dilatation and effacement are consequences of exposure of the chorioamnion membranes to microbial flora in the lower genital tract. The scan reveals a closed cervix and the presence of sludge in the same amount in the internal cervical orifice in a subset of patients (Figures 1 and 2). Chorioamnionitis represents the intra-amniotic infection and the risk factors are preterm rupture of membranes, prolonged labour, multiple vaginal exams, or vaginal colonization with various pathogens [3,4]. Histological classification of the placenta is considered the gold-standard for diagnosing; thus, we are talking about a retrospective diagnosis that is not useful in developing therapeutic management during pregnancy [5]. In our research, the placenta's acute inflammatory lesions were present in 60 percent of patients with preterm rupture of membranes and short cervix (Figure 4). Our study observed a robust association between sludge and intra-amniotic infection with preterm rupture of membranes and histological chorioamnionitis. At the histopathological examination, we observed that the placenta has vascularized, slightly hyperplasic chorionic villi, fibrinoid deposition, and rare dystrophic microcalcifications (Figure 3); amniotic membranes with acute inflammatory infiltrate with extensive necrobiosis; edematous diagnosis of severe acute necrotizing chorioamnionitis stage III, grade II.
References
Pisoh, D. W., Mbia, C. H., Takang, W. A., Djonsala, O. G. B., Munje, M. C., Mforteh, A. A., ... & Leke, R. J. I. (2021). Prevalence, Risk Factors and Outcome of Preterm Premature Rupture of Membranes at the Bamenda Regional Hospital. Open Journal of Obstetrics and Gynecology, 11(3), 233-251.
Danforth, D. N. (2008). Danforth's obstetrics and gynecology. Lippincott williams & wilkins.
Kachikis, A., Eckert, L. O., Walker, C., Bardají, A., Varricchio, F., Lipkind, H. S., ... & Brighton Collaboration Chorioamnionitis Working Group. (2019). Chorioamnionitis: Case definition & guidelines
for data collection, analysis, and presentation of immunization safety data. Vaccine, 37(52), 7610.
Kim JC, Romero R., Chaemsaithong P., Chaiyasit N, Yoon BH, Kim MY. Acute chorioamnonitis and funisitis: Definition, Pathologic features, and Clinical Significance. Am J Obstet Gynecol.2015;213(40):s29-s52
Tantengo OAG, Yanagihara I. Current understanding and treatment of intra-amniotic infection with Ureaplasma spp. The Journal of Obstet. Gynecology Research 2019; Vol. 45, No. 9:1796-1808